Definition
An elevation in the interstitial pressure in a closed osseofibrous compartment that results in microvascular compromise. Due to the unyielding stocking like aspect of the fascia large amounts of bleeding/swelling can cause large increases in the internal pressure of the compartment due to the minimal ability of the compartments to deform with the pressure.
Symptoms/Signs
The main symptoms and signs of compartment syndrome can be categorized by the “P’s”
- Pain out of proportion/Pain uncontrollable
- Pallor
- Pulseless
- Parasthesia
- Paralysis
- Pain with passive stretch
- Palpating firm compartments
While all symptoms may be present, early identification of the pain out of proportion and pain on passive stretch. Symptoms including pulselessness, parasthesia and paralaysis are late symptoms and often indicate a level of irreversible tissue damage.
Aetiology
- Commonly associated with fractures in long bones however compartment syndrome can still occur in patient with no fractures.
- Other potential causes include blunt contusion, haemorrhage into compartment, extravasation or reperfusion injury.
- Open fractures may not have large enough defect in fascia to prevent compartment syndrome. Therefore should be consideration in patient with open fractures as well.
- Often deteriorates as vicious cycle
- Increased tissue pressure causes increased compartment pressure which decreases tissue perfusion which causes ischemia which leads to cell death and release of myoglobin which increases compartment pressure.
Epidemiology
- Difficult to get a true value of incidence of compartment syndrome due to the low clinical suspiscion to treat. Fasciotomy for suspected compartment syndrome often acting as surrogate for incidence.
- Occurs at approximately 7.3 in 100,000 men and 0.7 in 100,000 women.
- Predominantly associated with fractures (~70%) with fractures of the tibia being the most frequent (36%), however other causes such as soft tissue injury without fracture still make approximately 30% of diagnosed compartment syndromes.
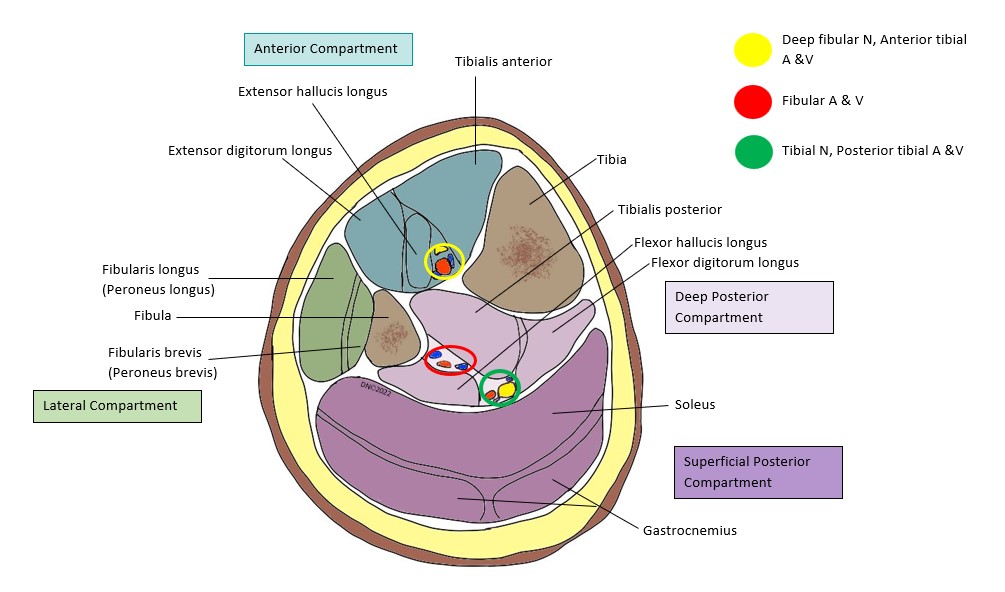
Anatomy
- Can occur in any part of of the body enclosed with fascia however commonly long bones including tibia/fibula, femur or forearm are most commonly affected.
- Deep fascia forms stocking like compartments surrounding the deep structures (muscle,bone,artery,nerve etc). This deep fascia is comprised of high levels of collagen fibre giving the fascia its strength. However this causes the deep fascia to have limited ability to expand with increased intracompartment pressure.
- Deep fascia surrounds individual muscle groups through intermuscular septa with pass between muscle groups and attach to underlying bone separating these muscle into specific compartments.
Compartment pressure
- Compartment pressure can be measured with a a pressure transducer (link to technique).
- Compartment syndrome diagnosed by measuring the delta pressure. The delate pressure is defined by the diastolic blood pressure minus the compartment pressure. If the delta pressure is under 30mmHg that suggests that the blood pressure is insufficient to perfuse distal tissue.
- This is however an uncommon investigative technique as often concerns for for compartment syndrome as treated early and aggressively or monitored closely clinically. Reasoning for starting compartment pressure monitoring may include
- symptoms of compartment syndrome confounded by other factors (eg neurologic injury, regional anaesthesia),
- increased firmness/swelling as only symptom in post op patient receiving regional anaesthesia
- unrealiable or unobtainable examination with firmness/swelling
- prolonged hypotension with swollen extremity with equivocal firmness
- spontaneous increase in pain in patient with adequate analgesia
Investigations
Radiological
- No formal radiological investigation exist for diagnosis of compartment syndrome
- However XR findings can increase suspicion (eg midshaft tibial fracture)
Biochemical
- Alongside routine bloodwork, serum lactate and creatinine kinase should be taken.
- While not diagnostic for acute compartment syndrome raised lactate and creatinine kinase can indicate an ongoing ischaemic process. Trends between serial blood changes can also be used to assess progress and decreases in both tests should be noted post treatment in an individual with nil other injuries.
Management of compartment syndrome
Initial management of compartment syndrome
- Splitting of casts and elevation of the limb is ideal initial as it is easy and quick management on the ward to help relieve some pressure in the compartment.
- Splitting all circumferential bandages & casts can ↓ compartment pressures by more than 50%.
- The optimal position for the limb is at heart level; this maximizes the arteriovenous gradient. Elevation above the heart decreases arterial inflow without altering venous outflow significantly.
Fasciotomy
- Surgical process where the fascia is split along the compartments to relieve pressure in the compartments
Fasciotomy for acute compartment syndrome of the thigh.
- Prep from iliac crest to knee.
- Make lateral incision from the trochanteric line to the knee lateral epicondyle. Incise the ITB in the line of the incision. Reflect vastus lateralis off the lateral intermuscular septum, & then divide the lateral intermuscular septum over the length of the wound.
- The pressure in the adductor compartment is then measured, & if elevated, it is released by a medial incision.
Fasciotomy for the leg (Double incision technique of Mubarak)
- Lateral incision 5-20 cm long, 2cm anterior to the fibula. Identify the SPN. Release the anterior & peroneal compartments through this incision.
- Medial incision 2cm posterior to the tibia, expose the deep & superficial posterior compartments & release these. Make sure the fascia over tibialis posterior is released. Caution for saphenous vein and nerve which sit posteriorly to incision site (superficial to deep fascia).
- Splint the foot in a plantigrade position.
Fasciotomy timing
- Fasciotomy is probably contraindicated if more than 3-4 days have gone by, as severe infection has been reported in patients who have their necrotic muscle exposed in this fashion.
Fasciotomy tips
- Important to identify any dead or necrotic tissue and remove/debride during the fasciotomy. Dead muscle can often be identified by the ease with which it is able to be removed by curettage. Muscle can be split to view deeper layers to ensure whole muscle is healthy and viable.
Complications
- Late treated compartment syndrome associated with severe morbidity and mortality. Due to the ischaemic and necrotic processes patients can become profoundly systemically unwell
- Local complications as well are common in late treated compartment syndrome with tissue death requring local amputation of the affected tissue as well less severe but chronic issues (neuralgia, muscular contractures (eg Volkmann’s contracture))
- Myoglobin release from breakdown of muscle also associated with increased risk of an acute kidney injury, thus appropriate hydration and monitoring of renal function is required.
References
Osborn, Col. Patrick M. MD; Schmidt, Andrew H. MD Management of Acute Compartment Syndrome, Journal of the American Academy of Orthopaedic Surgeons: February 1, 2020 – Volume 28 – Issue 3 – p e108-e114 doi: 10.5435/JAAOS-D-19-00270
Osborn PM, Schmidt AH. Diagnosis and Management of Acute Compartment Syndrome. J Am Acad Orthop Surg. 2021 Mar 1;29(5):183-188. doi: 10.5435/JAAOS-D-19-00858. PMID: 33337823.
Olson, Steven A. MD; Glasgow, Robert R. MD Acute Compartment Syndrome in Lower Extremity Musculoskeletal Trauma, Journal of the American Academy of Orthopaedic Surgeons: November 2005 – Volume 13 – Issue 7 – p 436-444
White T, Mackenzie S, Gray A, “McRae’s Orthopaedic Trauma and Emergency Fracture Management”, Third Edition, Elsevier, 2016
Author Contribution
Updated 2022 Dylan Ellis Resident
Image – Leg muscle compartments- Deepti Nayak 2022
