Western Health Orthopaedic Registrar presentation – Scaphoid Fractures by Dr Pandelis Dimitriou
Definition
- Fracture occurring through the scaphoid carpal bone of the wirst.
Aetiology
- Most commonly injured and fall, sports injury or vehicular accident
- A fall onto the outstretched hand with the wrist in ulna deviation causes the scaphoid to align with the axis of the radius causing a bending movement across the scaphoid
Epidemiology
- Most common fracture of the carpal bones accounting for 60-70% of all carpal bone fractures
- Prevalent predominantly in young males populations at an average age of 25 years, however females aged 10-14 were at the higher risk than older females
- Associated with Males > Females due to the increased participation in high risk activities in late teens to 30s
- Incident rates for Australia are ~40-50 per 100,000 for males and 8-15 per 100,000 females.
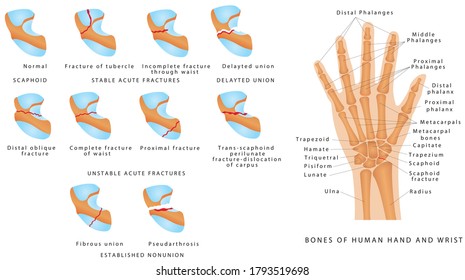
Anatomy
Osteology
- Most radial bone in proximal carpal row
- Curved structure described as resembling a “boat” or a “twisted peanut”. (Scaphoid is Greek for boat.)
- 75% of external structure is articulate cartilage.
- Articulates with radius, lunate, trapezium, trapezoid and capitate.
- Involved with stability and movement of wrist joint.
Vascular Supply
- The vascular supply of the scaphoid is important as scaphoid fractures of waist and proximal pole have a risk of avascular necrosis due to the distal insertion of its vascular supply
- Blood supply enters scaphoid through distal pole
- Dorsal side from dorsal ridge
- From dorsal branch of radial artery
- Supplies proximal scaphoid through retrograde flow
- Volar side from Distal Tubercle
- From superficial palmar branch of radial artery
- Supplies distal 1/3 of scaphoid
- Dorsal side from dorsal ridge
Pathology
- Most common fracture occurring across the waist of the scaphoid (~70 %)
- Fractures across distal third account for ~20% with proximal third ~10%
Classification
- Two commonly used classification systems for scaphoid fractures are the modified Herbert classification System and the Mayo (Cooney) classification system.
Modified Herbert Classification
Fracture classification based on stability of fracture pattern (A or B) and location.
| Type | Fracture Pattern |
|---|---|
| Type A1 | Stable fracture, through tubercle of scaphoid |
| Type A2 | Stable fracture, incomplete through scaphoid waist |
| Type B1 | Unstable fracture, distal oblique |
| Type B2 | Unstable fracture, complete fracture through scaphoid waist |
| Type B3 | Unstable fracture, proximal fracture |
| Type B4 | Unstable fracture, trans-scaphoid peri-lunate fracture/dislocation of carpus |
| Type C | Delayed Union |
| Type D | Non union (fibrous, pseudoarthrosis etc) |
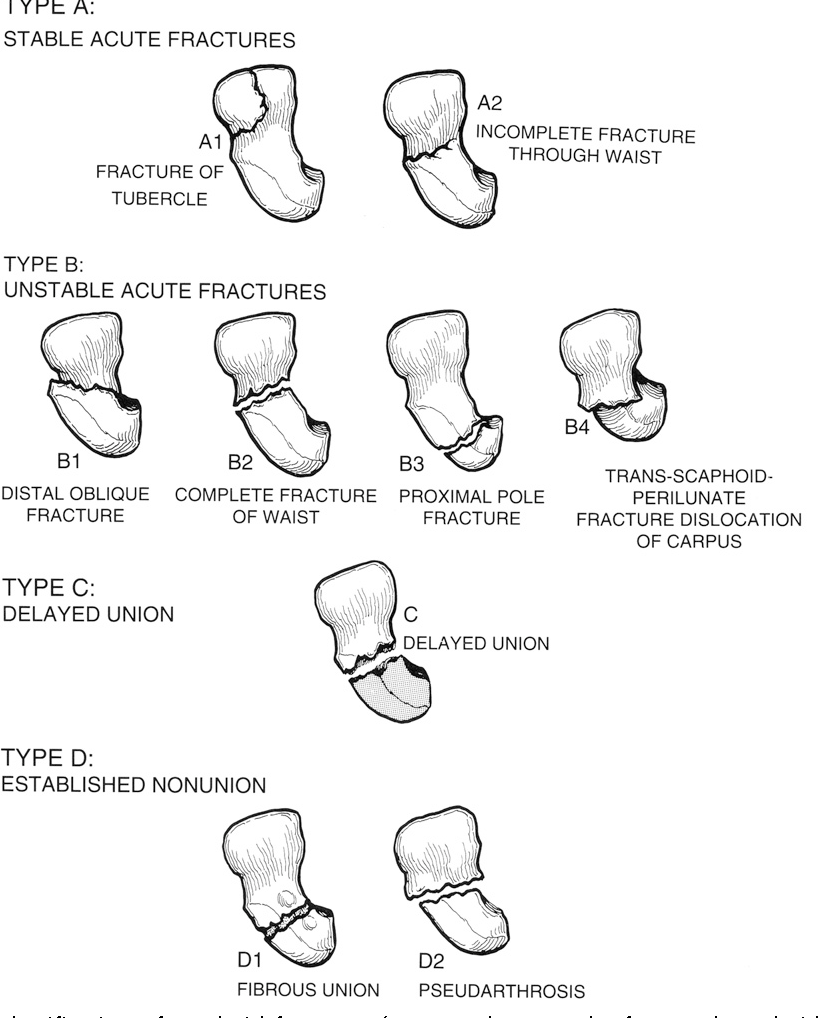
https://www.semanticscholar.org/paper/Acute-scaphoid-fractures.-AdamsSteinmann/2856d7ecde71b69ad8ba879466050b6590dd7046/figure/0 (From Quality Medical Publishing; 1990)
Mayo Classification
- Fracture classification based on location of fracture and guideline for determining stability of fracture pattern and characteristics.
5 primary locations of scaphoid fractures

Type 1: Distal Tubercle
Type 2: Distal Intra-articular surface
Type 3: Distal Third
Type 4: Waist
Type 5: Proximal pole
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4838473/figure/FI1500090-2/ (STM guidelines, from Cooney et al)
| Stable Fracture | Unstable Fracture |
|---|---|
| Displacement <1mm | Displacement >1mm |
| Normal intercarpal alignment | DISI Alignment (Dorsal Intercalated Segmental Instability) |
| Capitate- Lunate Angle: 0 to 15 degrees | Capitate- Lunate Angle: >15 degrees |
| Scaphoid Lunate Angle: 30 to 60 degrees | Scaphoid Lunate Angle >60 degrees |
| Lateral Intrascaphoid Angle <35 degrees | Lateral Intrascaphoid Angle >35 degrees |
| Distal Scaphoid Fracture | Comminuted or Perilunate Fractures |
History
- Fall onto an outstretched hand,
- often associated with high risk activities (eg. sports) however should be considered in low force falls as well
- Pain in wrist joint , worst in area of anatomic snuffbox
- Pain levels can be variable, not all scaphoid fracture present with severe pain and can be easily misdiagnosed as a sprain
- Pain may be most severe on movement of thumb
Examination
Inspection
- Swelling of wrist
- Rare to have deformity,
Palpation
- Anatomic snuffbox tenderness
- Scaphoid tubercle tenderness
Movement
- Pain on wrist movement
- Pain on axial compression of thumb
Anatomic snuffbox tenderness, scaphoid tubercle tenderness and axial compression of thumb are most commonly used tests to assess for scaphoid fracture. Done together sensitivity for the tests reach close to 100% and specifity at 74%.
Investigations
Radiologic
XR
- Wrist XR w scaphoid views (AP/Lateral/Oblique/30 degree wrist extension, 20 degree ulnar deviation).
- Must ensure that scaphoid XR views are taken. Due to the complex shape of the scaphoid, fractures may be missed on standard AP/Lat XR views.
- Best early investigation however may be non diagnostic in around 30% of scaphoid fractures. Therefore radiographic views can’t replace proper examination and clinical suspicion.
- If early radiographic views are negative then clinical examination with repeat XR at 10-14 days can be used to identify occult fractures.
CT
- Best modality to assess characteristics of fracture including displacement. Scaphoid fractures identified on XR should be considered imaging with supplementary CT to assess fracture pattern and displacement.
- Able to identify non union/malunion.
- Not as sensitive/specific as MRI but can be used to help identify occult fractures in situations where MRi is unavailable.
MRI
- Most investigation to identify occult fracture ~99% sensitivity/specificity. Gold standard for diagnosis of scaphoid fractures.
- Best at identifying ligamentous injury associated with fracture.
- T1 Weighted MRI able to identify vascularity of scaphoid (particularly proximal pole) and assess for AVN.
Bone Scan
Differential Diagnosis
- Distal Radius Fracture
- Metacarpal Fracture excluding scaphoid
- Wrist Strain/Sprain
Treatment
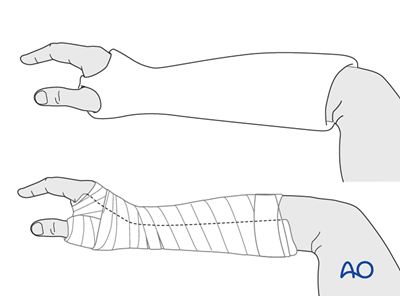
Non Surgical
- Appropriate for tuberosity fractures, incomplete fractures, displaced waist fractures or scaphoid fractures in low demand or high risk patients.
- Cast immobilisation for minimum 6 weeks for tubercle fractures and 8-12 weeks for displaced waist fractures..
- CT should be considered to properly identify fracture pattern level of displacement prior to cast immobilisation.
- Casting – Below elbow cast, wrist in slight extension, thumb in plaster in slight opposition.
- If clinical suspicion of a scaphoid fracture without definitive radiographic evidence, immobilisation and repeat XR at 10-14 days is warranted. This however may lead to over treatment of clinically diagnosed scaphoid fractures with only 5-20% demonstrating any radiological evidence at the 10-14 day mark. Immobilisation with MRI is also acceptable for diagnosis of occult fracture being highly sensitive and able to identify fractures immediately after the injury.
Surgical
- With fixation, healing is quicker and cast immobilisation time is decreased.
- Difficulties with surgical fixation include the complex curved shape of the scaphoid and high percentage of articular cartilage on the surface of the scaphoid.
Percutaneous Screw Fixation
- Indicated for undisplaced or minimally displaced scaphoid fractures
Open Reduction Internal Fixation
- Warranted for scaphoid fractures unable to reduced closed.
- Can be done via the volar traction-assisted approach; the dorsal minimal incision approach, with manual reduction as the guidewire is advanced; or the dorsal approach with arthroscopy-assisted reduction
Surgical Technique
Complications
- Non- Union
- Avascular necrosis/Osteonecrosis
- Dorsal Intercalated Segment Instability (DISI)
- SNAC (Scaphoid non-union advanced collapse)
Prognosis
- Early identification and treatment is associated with good outcomes. However delays in treatment can lead to increased risk of malunion. Delays of up to 3-4 weeks can dramatically increase the risk of scaphoid non union.
- Distal scaphoid fractures have often better clinical outcomes than proximal pole fractures with increased risk of AVN and non union.
References
- Berg, P.W., Drijkoningen, T., Strackee, S., & Buijze, G. (2016). Classifications of Acute Scaphoid Fractures: A Systematic Literature Review. Journal of wrist surgery, 5 2, 152-9 .
- Clementson M, Björkman A, Thomsen NOB. Acute scaphoid fractures: guidelines for diagnosis and treatment. EFORT Open Rev. 2020;5(2):96-103. Published 2020 Feb 26. doi:10.1302/2058-5241.5.190025
- Fox MG, Gaskin CM, Chhabra AB, Anderson MW. Assessment of scaphoid viability with MRI: a reassessment of findings on unenhanced MR images. AJR Am J Roentgenol. 2010 Oct;195(4):W281-6. doi: 10.2214/AJR.09.4098. PMID: 20858790.
- Garala K, Taub NA, Dias JJ. The epidemiology of fractures of the scaphoid: impact of age, gender, deprivation and seasonality. Bone Joint J. 2016 May;98-B(5):654-9. doi: 10.1302/0301-620X.98B5.36938. PMID: 27143737.
- Gutow, Andrew P. MD Percutaneous Fixation of Scaphoid Fractures, Journal of the American Academy of Orthopaedic Surgeons: August 2007 – Volume 15 – Issue 8 – p 474-485
- Holloway KL, Moloney DJ, Brennan-Olsen SL, Kotowicz MA, Bucki-Smith G, Morse AG, Timney EN, Dobbins AG, Hyde NK, Pasco JA. Carpal and scaphoid fracture incidence in south-eastern Australia: an epidemiologic study. Arch Osteoporos. 2015;10:10. doi: 10.1007/s11657-015-0215-6. Epub 2015 Apr 25. PMID: 25910867.
- Matej Kastelec, Renato Fricker, Fiesky Nuñez, Terry Axelrod, https://surgeryreference.aofoundation.org/orthopedic-trauma/adult-trauma/carpal-bones
- Simonian, Peter T. MD; Trumble, Thomas E. MD Scaphoid Nonunion, Journal of the American Academy of Orthopaedic Surgeons: July 1994 – Volume 2 – Issue 4 – p 185-191
- Ring, David MD; Jupiter, Jesse B. MD; Herndon, James H. MD, MBA Acute Fractures of the Scaphoid, Journal of the American Academy of Orthopaedic Surgeons: July 2000 – Volume 8 – Issue 4 – p 225-231
- Ten Berg PW, Drijkoningen T, Strackee SD, Buijze GA. Classifications of Acute Scaphoid Fractures: A Systematic Literature Review. J Wrist Surg. 2016;5(2):152-159. doi:10.1055/s-0036-1571280
- Trumble, Thomas E. MD; Salas, Peter MD; Barthel, Traci MD; Robert, Kearny Q. III MD Management of Scaphoid Nonunions, Journal of the American Academy of Orthopaedic Surgeons: November 2003 – Volume 11 – Issue 6 – p 380-391
Author Contribution
2021 Dylan Ellis – Orthopaedic Resident
