Anatomy

Unstable 4 part Pertrochanteric NOF
Bony
Normal
- neck shaft angle → 130° ± 7°
- femoral anteversion → 10° ± 7°
- Femoral head diameter → 40 to 60mm
- cartilage thickness → 4mm tapering to 3mm on the periphery.
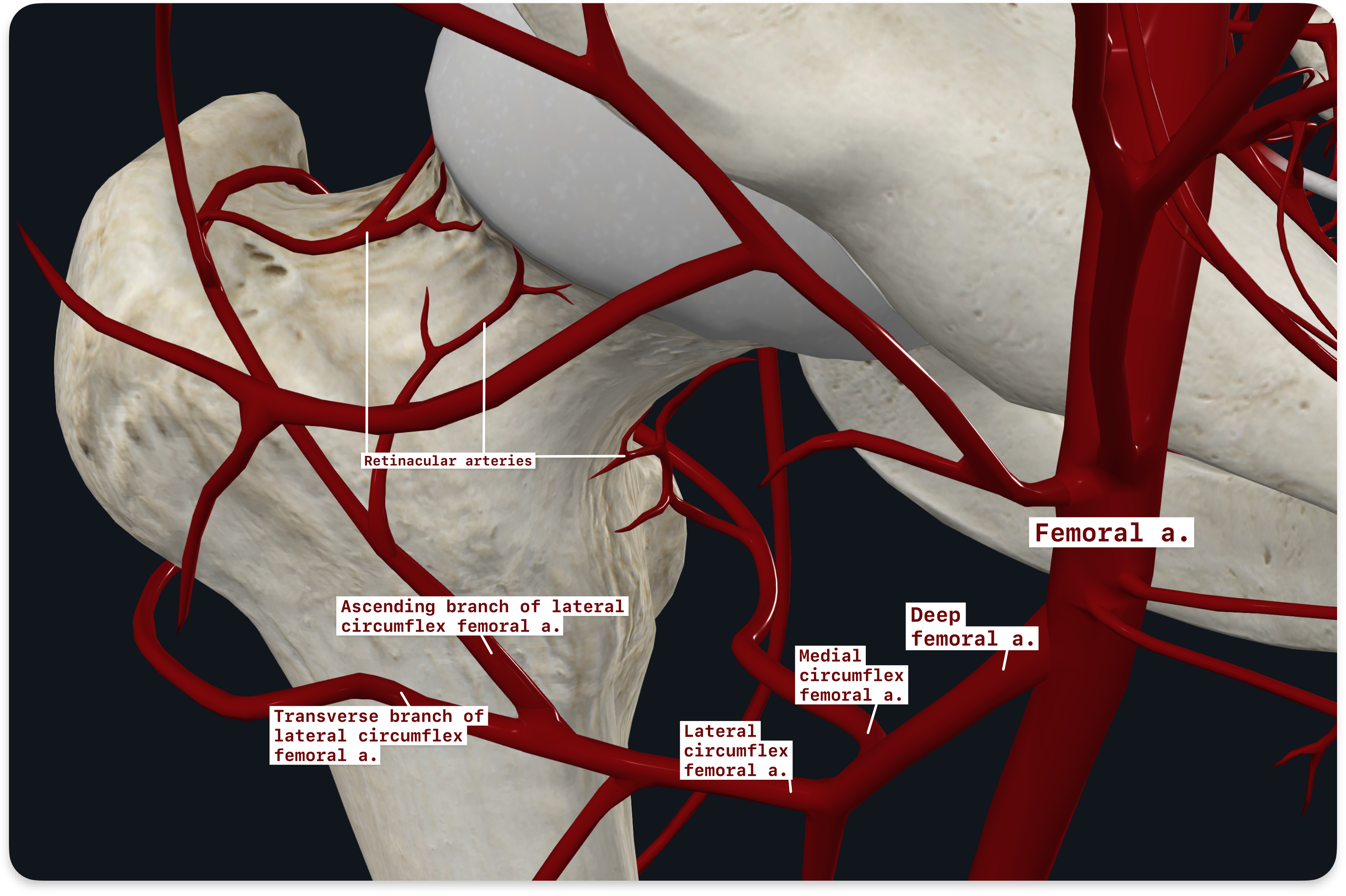
Vascular
The arterial supply to the femoral head
- three sources
- Endosteal arteries
- round ligament
- (ligamentum teres, a branch of the obturator or medial circumflex artery).
- This is significant in only around 1/3.
- also known as the medial epiphyseal vessels.
- extracapsular vessels.
- arise predominantly from the medial circumflex femoral artery, a branch of the profunda femoris
- lies just underneath the proximal margin of the quadratus femoris.
- A lesser contribution comes from the lateral circumflex femoral artery
- arise predominantly from the medial circumflex femoral artery, a branch of the profunda femoris
- Extracapsular Arterial Ring
- These two arteries ( MCFA & LCFA) give rise to an extracapsular arterial ring
- located at the base of the femoral neck.
- ascending cervical arteries arise from this ring
- also known as the retinacular arteries of Weitbrecht
- run upward beneath the capsule
- then underneath synovial reflections.
- most important branch is the lateral branch, known as the lateral epiphyseal artery.
- At the margin of the articular cartilage
- ascending cervical arteries form a subsynovial intraarticular arterial ring (so named by Chung).
- Epiphyseal branches arise from the ring that penetrate the head.
- These two arteries ( MCFA & LCFA) give rise to an extracapsular arterial ring
Epidemiology
- incidence doubles with every decade over 50.
- F:M 2-3:1
Risk factors
- Whites>blacks
- Urban dwellers
- Smokers
- Excessive alcohol or caffeine intake
- Physical inactivity
- Previous hip fracture
- Significant weight loss in midlife
- Use of psychotropic medication
- Senile dementia
- Postmenarche
- Institutionalization
- Osteoporosis
- Inadequate dietary calcium intake
Aetiology
- High violence injury in young patients
- Low violence injury in older patients (over 50).
- Hip protectors may be protective, particularly in nursing home patients.
Classification
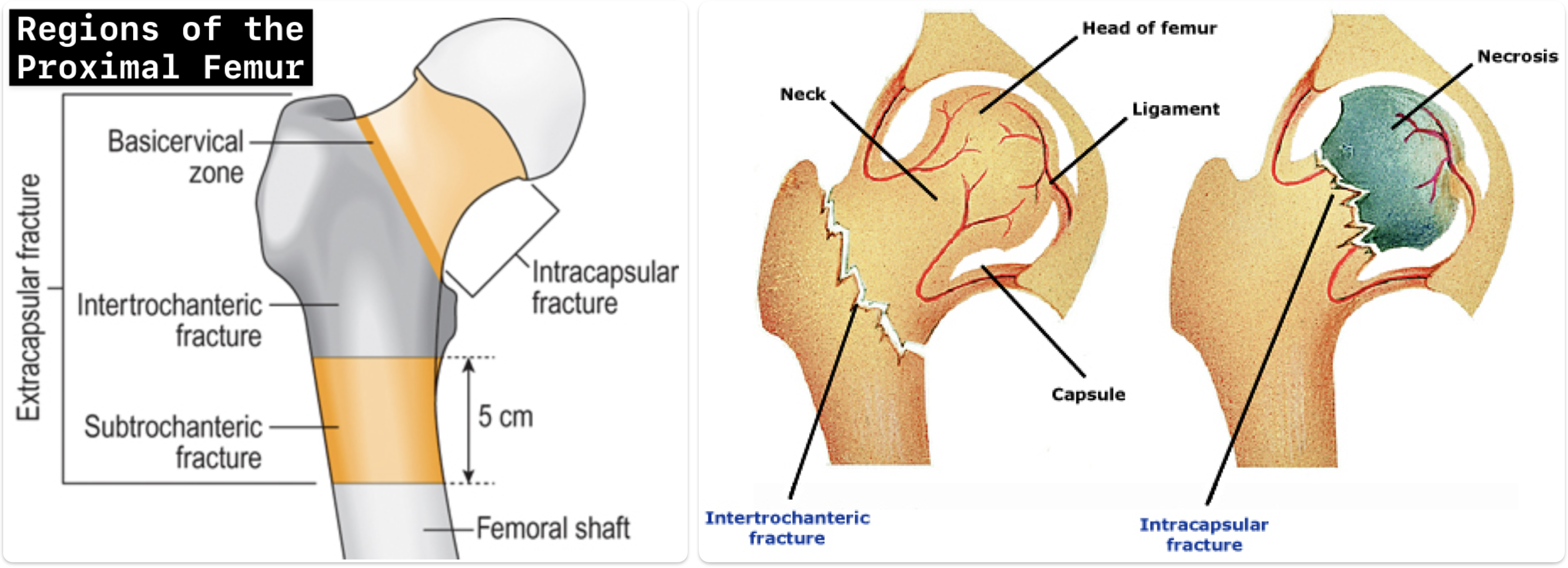
Hip fractures are classified by anatomic location and by fracture type. The general categories include:
- Intracapsular (femoral head and neck) – for reasons discussed above, intracapsular fractures have a higher rate of nonunion or malunion and are more likely to lead to avascular necrosis of the femoral head.
- Extracapsular (intertrochanteric and subtrochanteric) – extracapsular is defined as extending from the extracapsular femoral neck to the area just distal to the lesser trochanter. || Subtrochanteric fractures have an ↑ need for implant devices, such as intramedullary nails (or rods) and have higher rates of implant failure due to the high stresses placed upon this part of the femur.
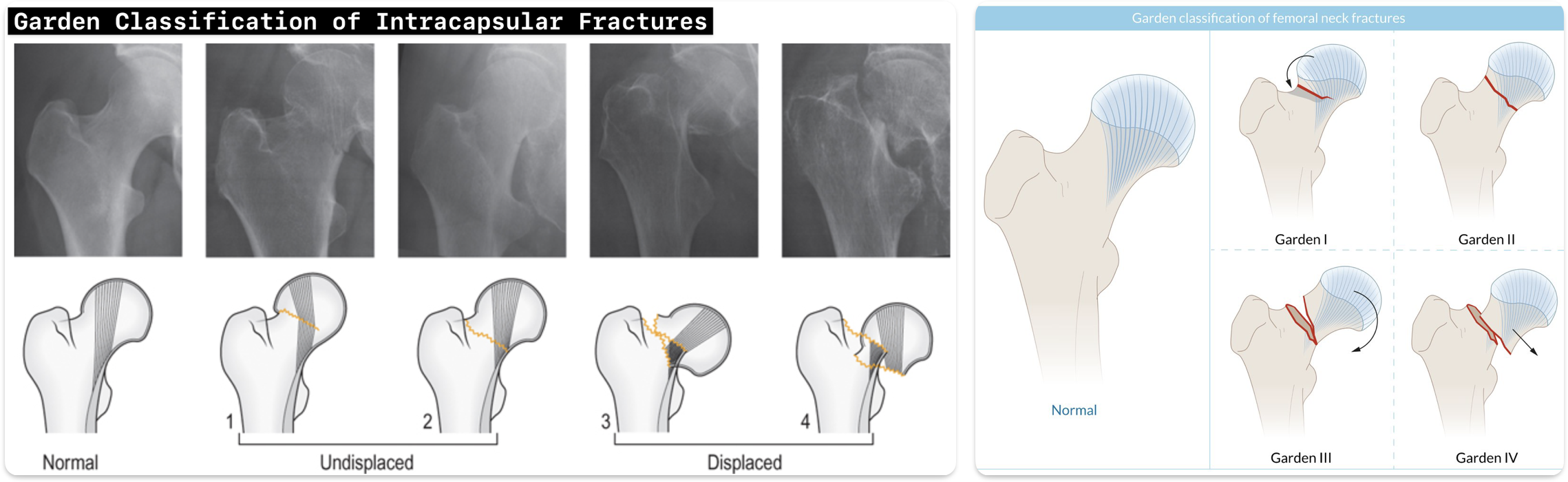
Classification of Intracapsular Fractures
The GARDEN CLASSIFICATION describes four patterns of intracapsular fracture, as seen on the AP radiograph:
- Garden 1: The fracture is valgus impacted (i.e. the apex of the fracture points medially). Classically, the medial cortical fracture is not seen on the radiograph.
- Garden 2: The fracture is complete but undisplaced, and the trabeculae remain aligned.
- Garden 3: The fracture is moderately displaced with disturbance of the trabecular pattern (displaced <50% and in varus)
- Garden 4: The fracture is displaced but the trabeculae line up to indicate that the head lies in neutral rotation (completely displaced).
In practice, it is neither possible nor very useful to differentiate between these four types consistently or reliably. However, identifying displacement (and therefore the likelihood of retinacular vessel disruption) is crucial.
- Garden 1 and 2 fractures are best termed ‘undisplaced’.
- Garden 3 and 4 are ‘displaced’.
The Garden classification does not take into account the displacement, usually posterior tilt, that may be present on the lateral hip radiograph. Although there is no current consensus, a hip fracture with a posterior tilt of >10° should be viewed as displaced.
Classification of Extracapsular Fractures
Extracapsular fractures include basicervical, intertrochanteric and subtrochanteric types:
- Basicervical fractures occur at the base of the femoral neck, but are extracapsular and do not impair the blood supply to the femoral head.
- Intertrochanteric fractures are the most common. Both the terms intertrochanteric and pertrochanteric are frequently used, and although they do have subtly different meanings (the fracture line in the former passes transversely below the greater trochanter and above the lesser trochanter, whereas in the latter the fracture line passes obliquely from one trochanter to the other), they are often used interchangeably.
- Subtrochanteric fractures originate in the 5 cm distal to the lesser trochanter. They account for only 5% of extracapsular fractures but are considered separately because of their biomechanical characteristics. Pathological metastases have a predilection for the subtrochanteric region. In addition, a small proportion of low-energy subtrochanteric fractures are termed ‘atypical fractures’.
- The method of fracture fixation is dependent on the fracture pattern and its inherent stability. There is no useful single classification system, although various modifications of a classification by Evans have been proposed (see below).
Investigations
- MRI
- more cost effective than bone scanning in detecting occult femoral neck fractures.
Prevention of thromboembolic disease
- There is at least a 40% rate of TED in hip fracture patients without prophylaxis.
- Subcutaneous LMWH has been shown to be an effective prophylaxis in patients with hip fracture.
- Subcutaneous heparin has not been shown to be effective.
- Lancet trial showed low dose aspirin was superior to placebo in preventing fatal PEs in hip fracture patients.
Functional recovery
- 40-60% of elderly patients with hip fractures are able to return home immediately after hospitalization.
- 10-20% become nonambulatory in the first year after fracture.
Mortality
- 1 year mortality rate
- 14 to 36%
- higher than in age matched controls.
- majority of deaths occurs in the first 4-6 months
- Once the patients get to 1 year their mortality parallels their peers without fractures.
- 50% of patients with femoral neck fractures survive 5 years.
- lowest mortality rates are in community dwellers without dementia.
- Institutionalized patients with severe dementia have in hospital mortality rates of up to 50%.
- A surgical delay of more than 3 days approximately doubled the risk of death before the end of the first postoperative year.
- Delay is only acceptable to stabilize medical conditions.
- Use of spinal vs. general anaesthesia doesn’t appear to affect mortality.
- mortality rate is slightly higher in patients treated with THR than with internal fixation in the first month, but by 3-4 months mortality is equivalent.
Example Case Histories
- A 72-year-old woman presents with a history of a fall from standing height and an inability to bear weight afterwards. She reports pain in her right hip. There were no preceding syncopal episodes and no loss of consciousness or chest pain. Physical examination reveals that her right hip is painful and sore to palpation with some ecchymoses over the greater trochanter. There are no breaks in the skin, and the right leg is shortened and externally rotated. The pelvis is stable clinically, and there is no pain along the spine and no deformity along the femoral shaft, knee, or tibia. The distal neurovascular status is intact. Cardiac and pulmonary examination is normal.
- Usually occurs in patients aged >65 years or in those who have osteopenic conditions of bone or osteoporosis. They are generally due to low-energy injuries in this patient group. However, hip fractures may present in younger patients with high-energy injuries such as motor vehicle accidents and falls from a height; these fractures can then be associated with other fractures of the femur and other injuries consistent with poly-trauma. Hip fractures may also be related to metastatic bone disease or rarely a primary bone tumour.
