Definition
- Also referred to as a high ankle sprain
- Involves one or more ligaments of the distal tibiofibular syndesmosis
Aetiology
- Inversion trauma
- External rotation injuries is the most common mechanism
- Talus rotates laterally, widening the space between the tibia and fibula
Epidemiology
- Difficult to have an exact incidence because it depends on the mode of diagnosis (clinical, versus radiological) used by the study.
- Occurs in ~13% of ankle fractures
- Occurs in ~6% of ankle sprains without fracture
- Common in sports injuries
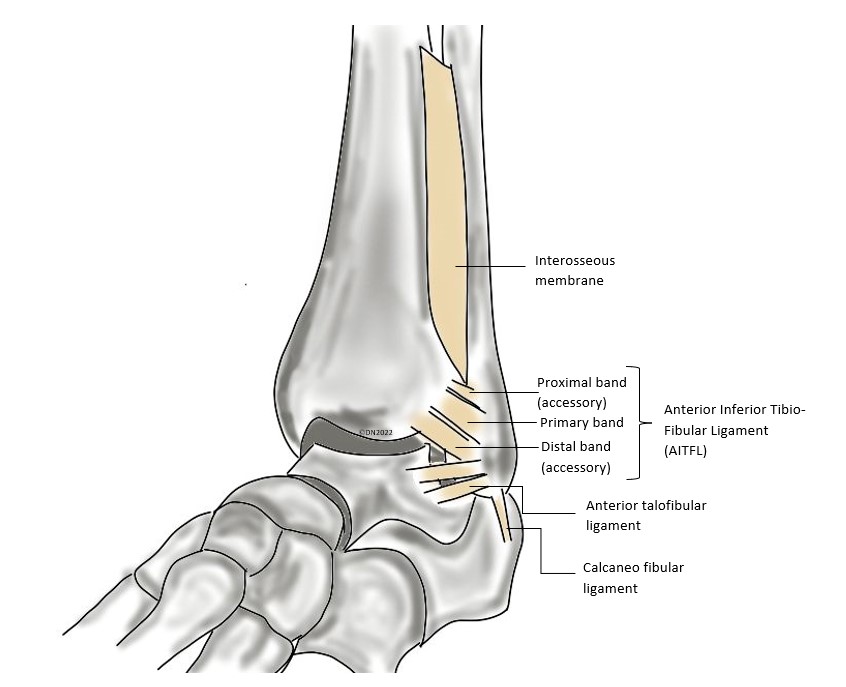
Anatomy
| Lateral | Medial |
| Anterior talofibular ligament Posterior talofibular ligament Calcaneal fibular ligament Lateral talocalcaneal ligament Syndesmosis: – Anterior inferior talofibular ligament – limits fibular external rotation – Posterior inferior talofibular ligament – prevents posterior fibular translation – Transverse talofibular ligament – limits posterior talar displacement – Interosseous ligament – limits lateral translation of the fibular | Deltoid: – Posterior tibiotalar – Tibiocalcaneal – Anterior tibiotalar Calcaneonavicular (spring ligament) |
Classification systems
As per the European Society of Sports Traumatology, Knee Surgery and Arthroscopy-Ankle and Foot Associates consensus panel, the most common classification for syndesmotic injury is divided into acute, subacute and chronic.
Acute (<6 weeks):
- Stable – injured AITFL +/- IOL, intact deltoid ligament
- Unstable – depends on other injuries including:
- Latent diastasis – injured AITFL, deltoid ligament +/- IOL
- MRI diagnosis
- Frank diastasis – injured all syndesmotic ligaments and deltoid ligament
- XR diagnosis
- Latent diastasis – injured AITFL, deltoid ligament +/- IOL
Subacute (6 weeks – 6 months)
Chronic (>6 months)
History
- Twisting like mechanism preceding the injury
- Anterolateral pain usually proximal to the AITFL
- Limp on weight bearing
- Medial tenderness + swelling
Exam
- Knee exam
- Ankle and Foot exam
- Pertinent findings: oedema not necessarily a feature (like it is for lateral sprains), antalgic heel raised gait, tenderness to palpation along AITFL
- Pay attention to syndesmosis tenderness on palpation + check for Maisonneuve fracture
- Special tests:
- Hopkins squeeze test -> compression at mid tibia region causes pain. Good specificity
- External rotation + dorsiflexion of foot with hip and knee at 90degrees causes pain at syndesmosis.
- Cotton test (stronger predictive value) – moving talus side-to-side with a neutral ankle. Increased translation with associated pain is a positive test. This is more likely completed in theatre as it is unlikely to be tolerated whilst the patient is awake.
- Fibular translation (stronger predictive value) à increased translation of the fibula + pain elicited when anterior and posterior drawer force applied to the fibula.
Investigations
- XRays (44-58% specificity)
- AP lateral and mortise views of ankle
- Unilateral wt bearing of the mortise view is best, however may not be tolerated by pt.
- AP lateral of fibula – ?Maisonneuve fracture
- Bilateral imaging
- Interpretation:
- Measure the distance between medial border of fibula and lateral posterior tibial prominence. This should be <6mm in anterior and mortise. If it’s more than this consider syndesmosis injury.
- Measure the overlap distance between the medial border of the fibula and lateral border of the distal tibia, should be more than 6mm in AP and 1 mm in mortise. If less than these consider syndesmosis injury.
- AP lateral and mortise views of ankle

- CT
- Normal Xrays, with ongoing clinical suspicion
- Weight bearing CT scan – assesses degree of instability
- MRI
- Normal XRays with ongoing clinical suspicion.
- Confirms ligament injury
- ~100% specificity
Differential diagnosis
- Lateral ankle sprain
- Maisonneuve fracture
- Weber fractures
Treatment
- Non-operative –> Rest, ice, elevate, NWB CAM boot or cast for 2-3 weeks, graded increase in physiotherapy exercises. Recovery time ~55 days
- Operative
- Indicated in syndesmotic sprain with instability (<6mm overlap b/w medial border of the fibula and lateral border of tibia, assoc fibula fracture)
- Unsuccessful non-operative management
- Post operative – period of non weight bearing (2-6 weeks), followed by focused rehabilitation and return to sports usually by 12 weeks
Surgical technique
- Screw fixation

- Suture button dynamic fixation
- Ligament reconstruction
Complications
- Post traumatic tibiofubular synostosis
- Degenerative ankle arthritis
Prognosis
- Favourable prognosis if identified and treated early
- Can lead to instability
Quiz
Review your knowledge about ankle syndesmosis injury via this short quiz
References
de-Las-Heras Romero J, Alvarez AML, Sanchez FM, et al. Management of syndesmotic injuries of the ankle. EFORT Open Rev. 2017;2(9):403-409. Published 2017 Sep 21. doi:10.1302/2058-5241.2.160084
Lin CF, Gross ML, Weinhold P. Ankle syndesmosis injuries: anatomy, biomechanics, mechanism of injury, and clinical guidelines for diagnosis and intervention. J Orthop Sports Phys Ther. 2006 Jun;36(6):372-84. doi: 10.2519/jospt.2006.2195. PMID: 16776487.
Schepers T, van der Linden H, va Lieshout EMM, Niesten DD, van der Elst M. Technical aspects of the syndesmotic screw and their effect on functional outcome following acute distal tibiofibular syndesmosis injury. Injury. 2014 Apr;45(4). doi: https://doi.org/10.1016/j.injury.2013.09.035
Shepherd D. Syndesmotic instability. Melbourne (AU): David Shepherd; 2022 [cited 5 Jan 2022]. Available from: https://drdavidshepherd.com.au/all-conditions/syndesmotic-instability/
Author Contributions
Francesca Sasanelli, created November 2021
