History
- Named after Jacques Lisfranc de Saint-Martin, a French field surgeon during the Napoleonic wars
Definition
- Involving the tarso-metatarsal joint (TMTJ)
- Broad spectrum of injuries
- Sprain or subluxation
- Fracture
- Fracture-dislocation
Epidemiology
- Approximately 0.2% of all fractures
- Accounts for more than 15% of all athletic injuries
- Second most common athletic injury
- Occurs most frequently in third decade of life
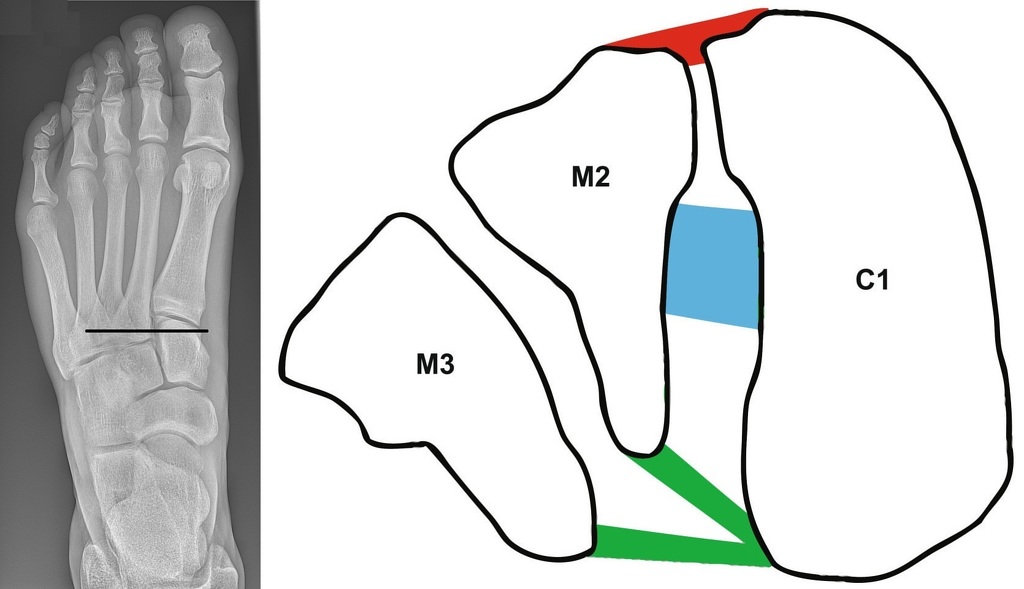
Anatomy
Bony Stability
- Midfoot made up of 5 bones
- navicular, cuboid, 3 cuneiforms
- Lisfranc joint comprised of 3 cuneiforms, cuboid and 5 metatarsals (MT)
- 1st to 3rd MT articulate with cuneiforms
- 4th and 5th MT articulate with cuboid
- Bases of MT wider dorsally
- Form half of Roman arch
- 2nd MT is keystone of transverse arch
- 3 columns
- Medial
- medial cuneiform and 1st MT
- Middle
- intermediate and lateral cuneiforms and 2nd and 3rd MT
- Lateral
- Cuboid and 4th and 5th MT
- Medial
Ligamentous Stability
- Dorsal, plantar and interosseous ligaments
- Longitudinal, oblique and transverse fibres
- LisFranc ligament
- 1cm x 0.5cm
- Base of 2nd MT to medial cuneiform
- Isolated injury to this ligament results in instability
- Note: no intermetatarsal ligament from 1st MT to 2nd MT
Mechanism of Injury
High energy
- Twisting/abduction injury to forefoot
- Fall from horse with foot in stirrups
- MVA (most common)
- Axial loading
- Fall from height
- Ankle equinus with body weight loading
- Crush injury
- To dorsum of midfoot
- Greatest risk of compartment syndrome and open fracture
Low energy
- Professional athletic trauma
- Misstep (contributes to late diagnosis)
Classification
1. Myerson (most commonly used today)
- A: Total incongruity (lateral or dorsoplantar)
- B: Partial incongruity
- B1: medial displacement of 1st MT
- B2: lateral displacement of other MT
- C: Divergent displacement
- C1: partial
- C2: complete
2. Originally developed by Quenu and Kuss, modified by Hardcastle (less common)
- Homolateral
- All MT displaced in same direction
- Isolated
- Only 1st MT injured/displaced
- Divergent
- 1st MT displaced medially
- Other 4 MT displaced laterally
History and Examination
- Mechanism of injury
- High incidence of failure to diagnose
- Swelling and pain out of proportion
- Bruising plantar aspect of foot can indicate LisFranc ligament rupture
- Signs of compartment syndrome
Imaging
Radiographs
Non-weighbearing (NWB)
- AP
- Fleck sign
- Avulsion of LisFranc ligament from base of 2nd MT
- Assess medial column
- Fleck sign

- 30 degrees internal oblique
- Assess lateral column
- Lateral
Weightbearing (WB)/ stress radiographs
- If normal or equivocal findings on NWB but high clinical suspicion
- Diastasis between 1st and 2nd MT
CT
- Confirms displacement
- Identifies and assesses fracture pattern
MRI
- Primarily important for the diagnosis and management of low-energy Lisfranc injuries
- Can detect subtle marrow oedema
- Can potentially misdiagnose small avulsion fractures as bone bruise
Management
Non-operative
- For stable injuries with no displacement
- Non-displaced
- stable under radiographic stress exam
- Unusual to treat non-op
- Treatment
- NWM in cast
- Protected WB in controlled ankle motion walking boot
- Close serial follow up
Operative
- Indicated for any displacement
Closed technique
- For isolated LisFranc with diastasis
- Longitudinal traction
- Reduction 1st intermetatarsal joint
- Percutaneous fixation screws
- From medial cuneiform to 2nd MT
Open technique
- Several methods
- Open reduction internal fixation (ORIF)
- Open reduction with hybrid internal and external fixation (rare)
- Open arthrodesis (rare)
- One such technique described here
- ORIF
- 1st dorsal incision between 1st and 2nd MT, lateral to EHL
- Protect branches of superficial peroneal nerve (SPN)
- Reduce 1st and 2nd MT to cuneiforms
- Check AP reduction
- K wire provisional fixation
- 1st MT to medial cuneiform
- 2nd MT to intermediate cuneiform
- medial cuneiform to base 2nd MT
- +/- medial to intermediate cuneiform if unstable
- Cannulated screws over K wire
- 2nd incision between 3rd and 4th MT if required
- Reduce 3rd and 4th TMTJ
- K wire/screw 3rd MT to lateral cuneiform
- Fix 4th and 5th MT to cuboid with K wires
- 5th K wire usually inserted percutaneously
- Check oblique view
- Postop
- Strick NWB in early stages of healing
- Minimum 4 months before considering removal of hardware
Prognosis
- Residual pain and stiffness with non-anatomical reduction
- Secondary osteoarthritis
- Progressive planovalgus
References
Mulcahy, H. (2018). Lisfranc Injury. Radiologic Clinics Of North America, 56(6), 859-876. doi: 10.1016/j.rcl.2018.06.003
Richter, M., Wippermann, B., Krettek, C., Schratt, H., Hufner, T., & Thermann, H. (2001). Fractures and Fracture Dislocations of the Midfoot: Occurrence, Causes and Long-term Results. Foot & Ankle International, 22(5), 392-398. doi: 10.1177/107110070102200506
Author Contributions
Matthew Sun, medical student, Western Health Intern 2021
