Review based on:
Lee et al. Necrotizing Soft-tissue Infections: An Orthopaedic Emergency. J Am Acad Orthop Surg 2019;27: e199-e206
Background
- necrotising – to cause necrosis or flesh eating
- necrotising soft tissue infections – a spectrum of presentation
- technically infection of any or all of the soft tissue layers from skin to muscle
- necrotising fasciitis – a subset of these necrotising infections but is the most common (others include necrotising adipositis or necrotising pyomyositis)
- cf with non necrotising infections – Abx alone don’t work
Risk Factors
- diabetes – 71%
- IVDU – 43%
- others – smoking, trauma, previous MRSA infection, immunosuppression, age >60, renal failure
- Causative microbes:
- polymicrobial 75%
- common baceria – anaerobes (baceroides, clostridium), enterobacteriae (E coli, enterobacter, klebsiella, proteus)
- mono-bacterial – strep, MRSA, fungal
clostridia (gas gangrene) = most common monobacterial infection - fresh water – aeromonas hydrophilia
- sea water/oysters – vibrio vulnificans
Gas Gangrene
- secondary to clostrial infection (gram positive obligate anaerobe)
- historically thought to be a military disease (American Civil War, WWI (28% mortality), WWII (0.9% mortality), Vietnam War (0.016% mortality)
- combination of high velocity trauma, open wounds and presence of soil/spores
- more recently – China 2008, 2010 earthquakes, Haiti 2010 post earthquake
- Louis Pasteur/Joseph Lister – first people to realise the significance of bacterial infection in the aetiology of gas gangrene
WWI Experience
- WWI: centuries old soil deposited into bought to the surface by artillery and trench warfare
- Early years – anti-septic poured onto wounds
- Re-introduction of a Napoleonic practice by a Belgian doctor – ’debridement’
Pathophysiology
- must have a POINT OF ENTRY
- can be large or small (50% are not visible) but it is there
- ex fix pin sites, IV drips reported as access sites
- once in – rapid progression
- based on bacterial virulence factors
- cycle of tissue ischaemia, enzymatic degradation, cell lysis and a pro inflammatory systemic response
- local ischaemia limits access of IV ABx
Presentation
- variable – can be a vague or non descript presentation and sometimes it is difficult to cf between non necrotising infections
- pain out of proportion = best finding
- physical findings:
- initially benign
- erythema (red –> purple –> blue gray)
- oedema/welling
- induration of skin
- bullae – highly specific
- palpable crepitus
- most patients will be in septic shock

Hard Signs of Gas Gangrene
- anaesthesia
- ecchymosis/bullae
- gas in tissues
- NB: only if infection from species that grow under anaerobic conditions
Diagnosis
- should be a clinical diagnosis
- there are aids to help confirm this
- LRINIC calculator (look for it online) – a lab risk indicator (not validated) that helps determine PPV
- utilises CRP, WCC, Hb, Na, Cr and BGL
- score ≥8 = PPV 93.5% of Nec Fasc
- Can also use presence of gas in fascial planes on XR (but present only in a minority of cases)

Treatment
- indications for urgent surgery/debridement include CRP >150, WCC >25, metabolic acidosis/rising lactate
- a formal Dx of necrotising fascitis is only done once deep tissue cultures obtained
- MDT
- ABx – broad spectrum. JAAOS recommends Tazocin + Clinda + Vanc but best to involve ID
- no specific evidence based guidelines for Nec Fasc and ABx choice
- TPG in Aus suggests using Meropenem or Tazocin plus either Vancomycin/Clindamycin/Lincomycin
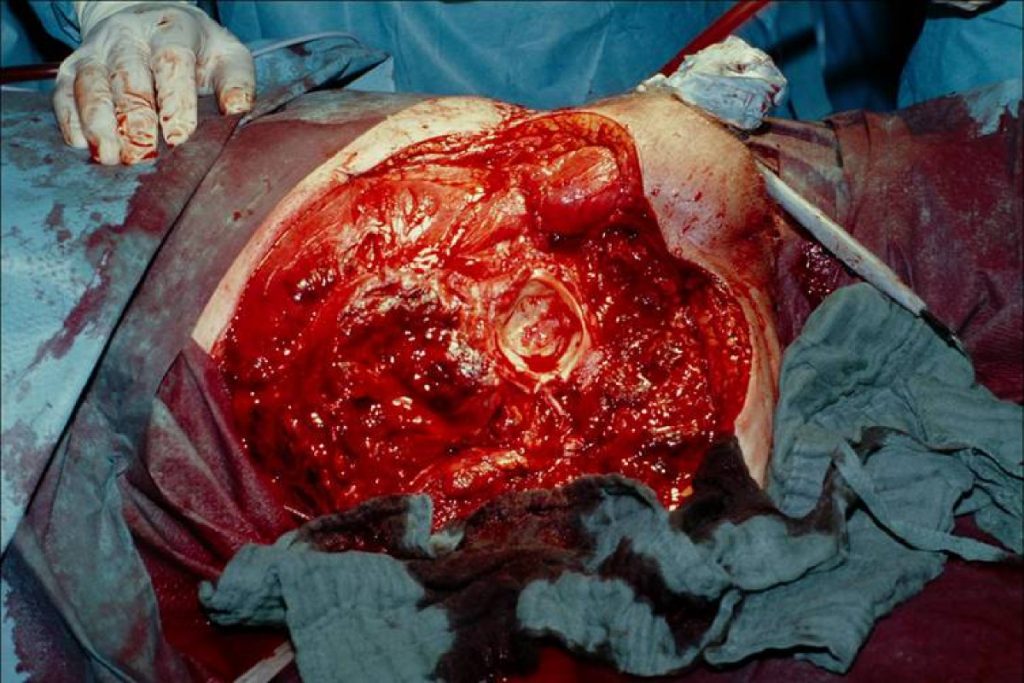
Debridement
- debride ASAP
- Expeditious soft tissue decompression of all necrotic tissue to healthy tissue with no regard for future reconstruction
- ABx
- commence with a longitudinal incision over the nidus of infection and extend proximally to healthy tissue
- often dual incisions required
- amputation an option – rapid progression where debridement alone is inadequate or the limb is non-salvageable
- temporary closure with VAC
- early surgical re-exploration after VAC closure after period in ICU
- average no of debridements usually 2-5x
Prognosis and Outcomes
- indicators of poor prognosis include bacteraemia, intravascular haemolysis, shock and visceral or truncal involvement
- occasionally, recurrent gas gangrene can occur in previous wounds that have previously been gangrenous
- high association with mortality (33%)
- risk factors for death same as risk factors for getting nec fasc in the first place
- surgical delay the single most modifiable risk factor
- amputation common – 18-28%
- however, improvement in outcomes over the past decade – probably secondary to early detection
