Definition
- The eponymously named ‘tennis elbow’ encapsulates the diagnosis of a lateral elbow tendinopathy or ‘Lateral Epicondylitis. This typically involves disruption of the tendon matrix of ECRB or ECRL, near the common extensor origin
Epidemiology
- The most common diagnosis for patients presenting with elbow pain, Affecting 1-3% of adults annually.
- Given its relationship to load, it typically occurs in the dominant hand.
- Peak incidence age 40 to 60
- Associated with high repetition sports requiring excessive gripping
- Associated with occupations requiring excess wrist extension
Anatomy and Physiology
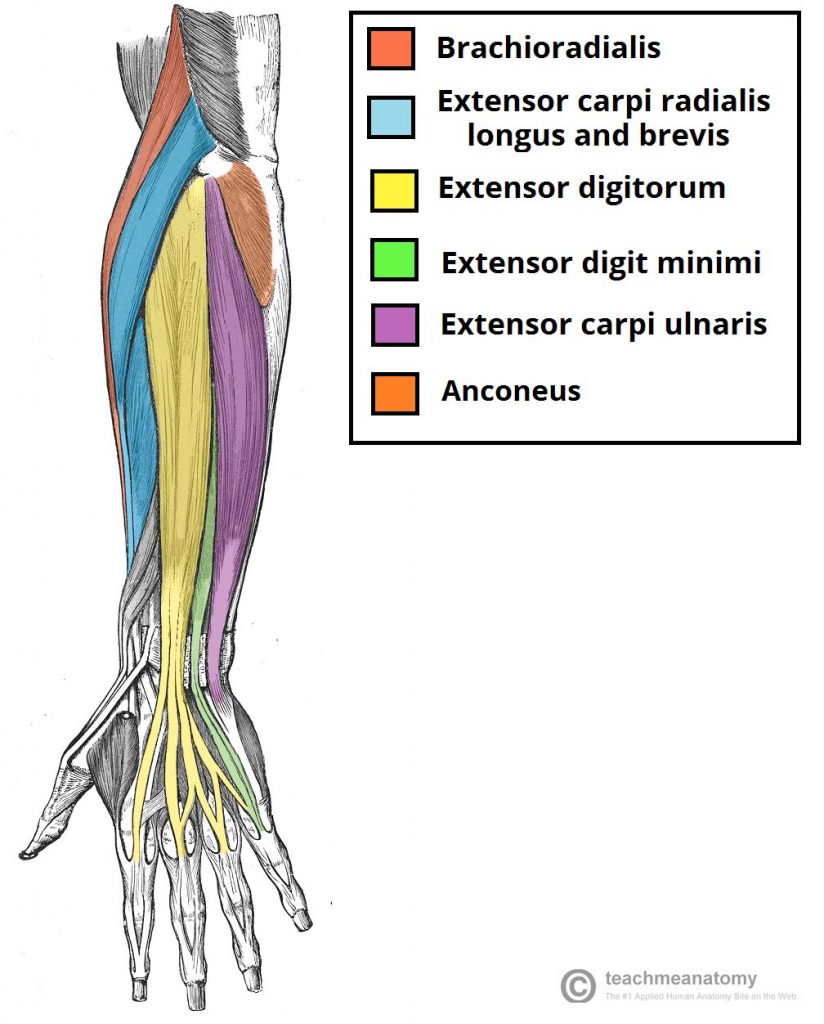
- Lateral elbow tendinopathy is cause by a tendinopathy of the extensor muscles which attach at the CEO (lateral epicondyle)
- The Extensor Carpi Radialis Brevis (ECRB) tendon is the most commonly affected tendon in elbow tendinopathy, followed by the Extensor Carpi Radialis Longus (ECRB).
- Tendinopathy is a relatively newly coined term that captures the lifecycle of a tendon as it responds to stress. There are typically thought to be 3 stages.
- Reactive tendinopathy
- A tendon responding to a sudden change in load, or an acute stressor (trauma). Localised inflammation, structurally remains intact and indectectable, with limited change to the tendon matrix or collagen integrity
- This is an entirely reversible and physiological process
- Dysrepair tendinopathy
- Following stage 1, if there remains to be excessive loading there will begin to be dysregulation of the collagen and tendon matrix, hypervascularity and neural ingrowth..
- Degenerative tendinopathy
- Chronic overloading condition, disorganised collagen, increased tendon matrix breakdown, further increased vasculairty and neural ingrowth. Thick and structurally weak tendons with a greater chance of tendon rupture.
Clinical Features
- The diagnosis of ‘tennis elbow’ is largely a clinical diagnosis, that requires very minimal investigation other than a comprehensive clinical examination. Further imaging is only necessary if there is doubt re diagnosis or if the injury is not responding well to exercise based therapy
- History
- Onset
- There are 2 clinical presentations of lateral elbow tendinopathy.
- The most common has an insidious onset 24-72 hours post activity unaccustomed to the patient involving repeated wrist extension (e.g laying bricks over weekend, using screw driver etc)
- Sudden onset elbow pain, in situation of single instance of exertion involving the wrist. The insidious onset is thought to correspond to larger macroscopic tendon tears.
- Activity type
- Activities of repetitive motion, requiring gripping or elbow extension e.g tennis, squash or occupation such as brick laying, sewing
- Change of activity:
- New physical activity or change in load to pre-existing exercise
- E.g hitting heavy tennis balls, poor technique in hitting ‘late’ requiring more forearm strength to compensate, change of raquet.
- Location of pain
- Typically 5cm distal to the lateral epicondyle
- Associated features
- Paraesthesia (typically radial nerve distribution), subjective feeling of weakness
- Onset
- Examination
- Look
- Joint deformity
- Inflammation
- Redness
- Feel
- Palpation at CEO (Lateral epicondyle)
- Insertional (at lateral epicondyle)
- Mid-substance lesion (typical 1-2cm distal of lateral epicondyle)
- Tissue tightness or hypersensitivity
- Move
- Reproducible pain namely on wrist extension when wrist is extended and forearm pronated.
- Particularly on Wrist extension (ECRB)
- Pronated and extended position is of the best sensitivity as ERCB also acts synergistically to anchor the 3rd MCP to allow extension to take place at the digits.
- Middle finger extension (ECRL)
- Neurovascular provocation test
- Radial nerve bias
- Cervical spine
- Typically decreased ROM lateral flexion at C-spine given radial nerve provocation testing.
Investigations
X-ray
- AP/Lateral view of elbow
- Would expect a normal XR, however, may show signs of calcification in the extensor musculature (minority of patients)
- Xray can assist in ruling out other differential diagnosis
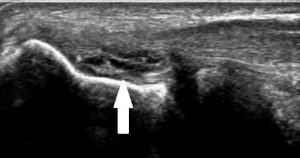
Ultrasound (Most diagnostic)
- The cavet of all US requires experienced ultrasonographer
- Increased thickness to extensor tendon, distortion of tendon architecture, hypo echoic appearance of tendon
MRI
- Limited utility
- Potential thickening, swelling and destruction of tissue architecture at extensor tendons.
Differential Diagnosis
- Septic arthritis
- Pseudogout
- Acute bursitis
- Cellulitis
- RA
- Osteoarthritis
- Seronegative spondyloarthropathy
Management
- No single treatment is totally effective, and like all orthopaedic injuries a multi-disciplinary approach is probably the most useful for patient.
- Goals of treatment
- Analgesia
- RICER (Rest, Ice, Compression, Elevation, Re-assess) in the early phase
- Bracing or Taping
- Bracing has been shown to increase forearm extensor stretch tolerance however does not improve strength or proprioception.
- De-loading taping (diamond taping technique) has been shown to reduce pain through reducing tissue stress.
- Isometric exercises
- Isometric wrist hold
- Medication (Paracetamol, NSAIDs, where appropriate)
- Electrotherapy (2nd line)
- Cortisone injection (2nd line) (usually if physiotherapy fails or pt unable to engage in exercised based strengthening due to pain)
- Injected to the point of most severe pain or around ERCB attachment site.
- Counsel pts that conservative therapy has a success rate of around 80% in 12 months.
- Platelet-rich plasma (last line) (PRP)
- Analgesia
- Address grip strength deficit initially through exercise based management
- Progressively graduated wrist strengthening exercises focusing on wrist extension primarily.
- Pain is expected during exercises, recommend exerting to 4-6/10 pain threshold.
- Manual based therapies can assist to assist in mobilisation, flexibility and engagement in further exercised based strenghting.
- Co-ordination based exercises
- Correction of pre-disposing factors
- Technique, equipment, jobs
- Return to function
Surgical techniques
- (Consider in those failing to respond to conservative management, or ongoing pain)
- Nirschl open release (with or without drilling)
- Incision around lateral epicondyle to expose ECRL, ECRB and EDC. Resection of the angiofibroblastic tendinosis tissue within ERCB
- Drilling – decorticating anterolateral humeral condyle, to increase blood supply. (Studies has recommend against, increased pain and nil increased patient benefit)
- Reported 85% success rate
- Median return to work 5 weeks
- One study showed, nil difference between (open release v sham surgery
- Percutaneous division of the common extensor origin
- Incision directly over lateral epicondyle, extensor origins divided transversely, incision though synovial membrane, decortication of bone at lateral epicondyle.
- Rest in sling 2 weeks, then early and active ROM exercises
- Nirschl open release (with or without drilling)
- Complications
- Surgical wound infections
- Haematoma
- Damage to nerve
- Need for revision surgery
REFERENCE
- Rees JD, Maffulli N, Cook J. Management of tendinopathy. The American journal of sports medicine. 2009 Sep;37(9):1855-67.
- Keijsers R, de Vos RJ, Kuijer PP, van den Bekerom MP, van der Woude HJ, Eygendaal D. Tennis elbow. Shoulder & elbow. 2019 Oct;11(5):384-92.
- Brukner P, Khan K. Clinical sports medicine revised. Australia: McGraw-Hill. 2002;128:145-72.